Diabetic Retinopathy

Image of diabetic retinopathy.
Diabetic retinopathy is a complication of diabetes that causes damage to the blood vessels in the retina. Diabetes affects the smallest blood vessels in the retina, the capillaries, which are located between arteries and veins. The capillaries may form small buds called microaneurysms which can leak fluid causing swelling (edema). The capillaries may also become blocked disrupting the blood supply of the retina. Finally, capillaries can grow abnormally causing neovascularization. These abnormal vessels are fragile can bleed without warning.
Exactly how elevated blood sugar leads to these changes in the retinal circulation is still being investigated. Nevertheless, control of blood sugar has been shown to delay or prevent the development of diabetic retinopathy. Other risk factors include the duration of diabetes, age, high blood pressure, high cholesterol and cigarette smoking.
Diabetic retinopathy is detected by a dilated examination of the retina. Regular eye examinations are important for anyone with diabetes, and should be done at least once a year. You may have diabetic retinopathy even though you have no visual symptoms. Fundus photography and fluorescein angiography are helpful in detecting and monitoring the progress of diabetic retinopathy. Optical Coherence Tomography can detect swelling of the retina before it is clinically apparent, and is very helpful in monitoring its progress.
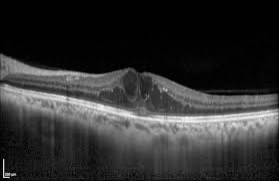
Image of diabetic macular edema using OCT.
The need to treat diabetic retinopathy depends on the activity of the retinopathy and how it affects your vision. If there is significant swelling of the retina (macular edema) treatment with either intravitreal injections or laser may be recommended. The injections are directed against vascular endothelial growth factor, a key mediator in growth of and leakage from blood vessels. Several drugs are currently available, and repeated injections are usually necessary to gain control of the macular edema. Steroid injections may also be used to control macular edema. Laser treatment of diabetic retinopathy has been available for over 50 years and is still quite effective in managing diabetic retinopathy. These treatments stabilize or improve vision in the majority of patients. Despite treatment, some patients may continue to lose vision as a result of diabetic maculopathy.